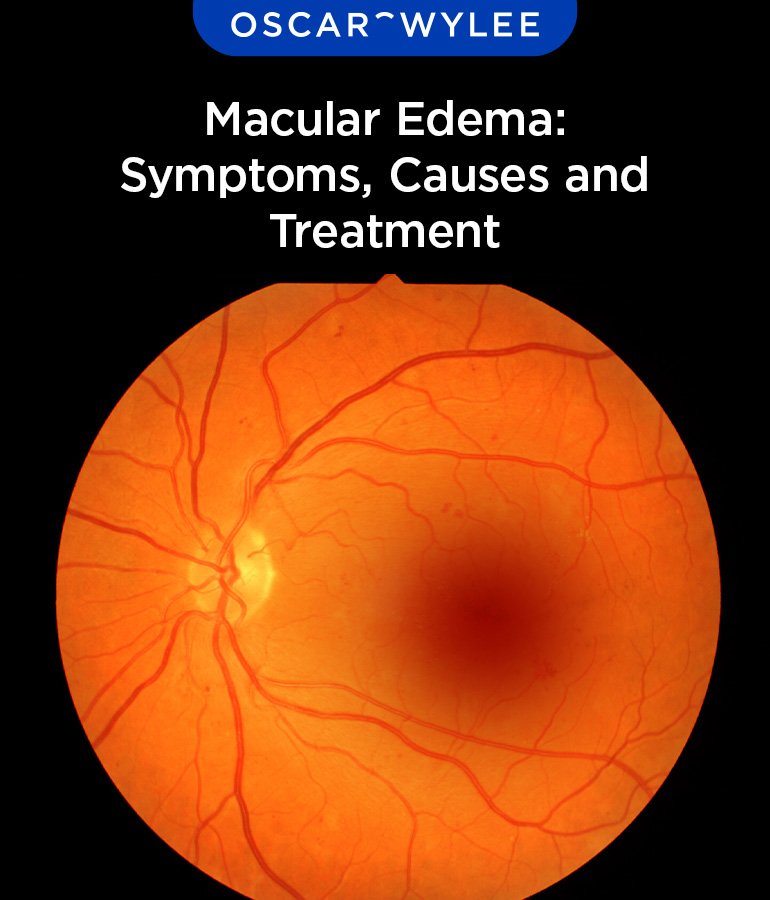
Macular edema and retinal edema are conditions that involve fluid buildup in the retina, leading to blurry vision and, in severe cases, vision loss. Macular edema specifically affects the macula, the part of the retina responsible for sharp central vision.
Table of Contents
One of the most common causes is diabetic macular edema (DME), which results from prolonged high blood sugar damaging retinal blood vessels. Other conditions, such as retinal vein occlusion, inflammation, and eye injuries, can also lead to swelling. Early detection and treatment are crucial in preventing permanent vision loss.
What is Macular Edema?
Macular edema occurs when fluid leaks into the macula, causing it to swell and distort vision. The macula, located at the back of the eye, plays a vital role in providing sharp, central vision.
A broader condition, retinal edema, refers to fluid accumulation anywhere in the retina. However, macular edema has a more direct impact on detailed vision, affecting daily activities such as reading, driving, and recognizing faces.
Causes of Macular Edema
Several conditions can lead to macular edema, with diabetes being the most common cause. High blood sugar levels damage the retinal blood vessels, leading to leakage and swelling, a condition known as diabetic macular edema (DME).
Other causes include retinal vein occlusion, where blocked veins cause blood and fluid to seep into the retina. Inflammatory diseases like uveitis or complications from eye surgery can also result in macular swelling. Additionally, age-related macular degeneration (AMD), as well as eye injuries, and certain genetic conditions contribute to fluid buildup in the macula.
Symptoms of Macular Edema
The symptoms of macular edema may develop gradually and worsen over time. Blurred or distorted vision is one of the earliest signs. Colors may appear faded, and some individuals experience increased sensitivity to light.
A common symptom is the appearance of dark or missing spots in the central field of vision. People may also find it difficult to adjust when moving between different lighting conditions. Since symptoms can be subtle at first, as well as regular eye exams are essential for early detection.
Risk Factors
Several factors increase the likelihood of developing edema. Uncontrolled diabetes is a primary risk, as prolonged high blood sugar damages retinal blood vessels. High blood pressure and cholesterol also contribute to poor blood vessel health, as well as raising the risk of fluid leakage.
Diagnosis
An eye doctor diagnoses edema through a comprehensive dilated eye exam, allowing them to examine the retina closely. Additional tests provide more detailed insights.
Corticosteroids
Steroids reduce inflammation in the retina and are delivered through injections or implantable devices that release medication over time. This treatment is effective for edema caused by inflammatory conditions. However, long-term steroid use may increase the risk of glaucoma or cataracts, as well as requiring careful monitoring.
Lifestyle Adjustments for Eye Health
Along with medical treatment, certain lifestyle changes can help manage macular and support overall eye health. Maintaining stable blood sugar, as well as blood pressure, and cholesterol levels is essential, especially for individuals at higher risk.
A diet rich in leafy greens, fish, and antioxidant-rich foods helps protect the retina from further damage. Regular physical activity improves circulation, as well as benefiting eye health and overall well-being. Avoiding smoking and excessive alcohol intake further reduces the risk of vision problems.
Routine eye check-ups remain the best way to detect macular changes early and prevent severe vision impairment. Following a doctor’s recommendations for managing underlying health conditions significantly improves outcomes for those with macular.